Note: Your progress in watching these videos WILL NOT be tracked. These training videos are the same videos you will experience when you take the full ProPALS program. You may begin the training for free at any time to start officially tracking your progress toward your certificate of completion.
Ventricular fibrillation (also called VFib or VF) is caused by multiple ectopic electrical impulses which depolarize the myocardium in a chaotic fashion. This results in a quivering (or fibrillatory) heart that cannot produce a pulse.
In this lesson, we'll dig a little deeper into ventricular fibrillation and then look at a typical ECG readout for a patient in VFib and provide a cardiac interpretation at the end.
Now let's take a look at an ECG for a patient in ventricular fibrillation.
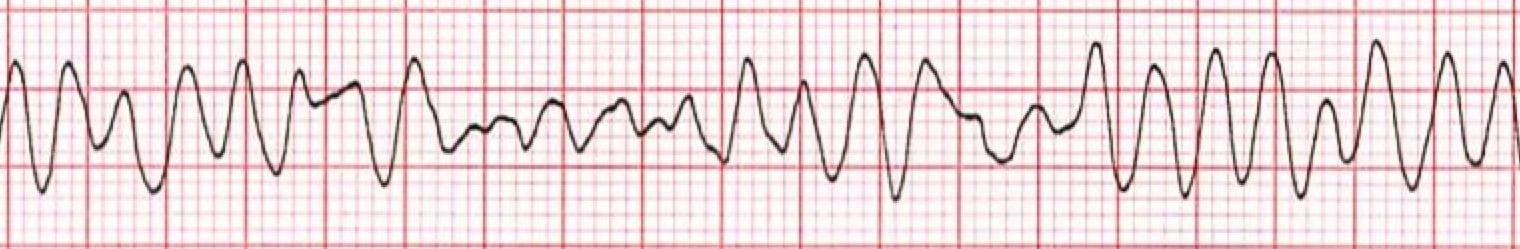
*Ventricular Fibrillation ECG
1. The Heart Rhythm
The first thing you'll want to look at is the heart rhythm. Does the heart rhythm look regular? Or does it look irregular? In the ECG above, the rhythm is irregular.
2. The Heart Rate
Next, you'll want to look at the heart rate of the patient. What is the patient's heart rate? Is it normal? Or is it too slow or too fast? In this case, there is no rate and no pulse.
3. P-Wave
After looking at the heart rate, check to see if the patient's P-waves look normal by asking yourself the following few questions.
- Are the patient's P-waves present? No.
- Do they occur regularly? No.
- Is there one P-wave for each QRS complex? No.
- Are the P-waves smooth, rounded, and upright? No, only fibrillatory waves are present.
- Do all the P-waves have a similar shape? Again, that answer is no, because normal P-waves aren't present.
4. PR Interval
Next, look at the PR interval on the patient's ECG readout and ask yourself the following questions:
- Is the PR interval normal, meaning less than .20 seconds or is it contained within one large square on the readout? The answer is no, because there isn't a PR interval.
- Is the PR interval constant? Again, this in non-applicable since there isn't a P-wave.
5. QRS Complex
The last thing you should look at to determine if the sinus rhythm is normal or not is the QRS complex and ask yourself these questions while you do:
- Is the QRS interval less than .09 seconds? No. In fact, there is no evidence of a QRS complex.
- Is the QRS complex wide or narrow? Not applicable.
- Are the QRS complexes similar in appearance or are there noticeable differences? Not applicable, since not present.
So, what is your cardiac interpretation? Based on these questions and on the findings from the ECG readout above, it would appear that this patient is in ventricular fibrillation.
- We have an irregular rhythm.
- We have no heart rate and no pulse.
- The P-waves are missing; there are only fibrillatory waves present.
- There is no PR interval.
- The QRS is nonexistent.
From the ECG alone, it would indicate that the patient is in VFib.
Pro Tip #1: VFib is a non-perfusing and lethal dysrhythmia that is most commonly seen during the first few minutes of cardiac arrest. Because of this, it's important that high-quality CPR be administered as soon as possible, including defibrillation, to increase that patient's chance of a successful resuscitation.
An Additional Word About Ventricular Fibrillation
When a patient is in ventricular fibrillation, the heart has no organized rhythm as well as no coordinated contractions. The electrical activity is very chaotic. The heart quivers and it does not pump blood. Therefore, pulses are not palpable. Ventricular fibrillation may be preceded by a brief period of ventricular tachycardia with or without a pulse.
Primary ventricular fibrillation is not common in children. In studies involving pediatric cardiac arrest, VFib was the initial rhythm in between 5 to 15 percent of both out-of-hospital cardiac arrests (OHCA) and in-hospital cardiac arrests (IHCA).
The overall prevalence may be higher because VFib can occur early during cardiac arrest and quickly deteriorate to asystole. VFib has been reported in up to 27 percent of pediatric in-hospital arrests at some point during the resuscitation.
VFib without a previously known underlying cause is rare but can sometimes occur in otherwise healthy teens during sports activities. The cause of VFib can also be due to an undiagnosed cardiac abnormality or channelopathy, such as long QT syndrome – a heart rhythm condition that can potentially cause fast and chaotic heartbeats.
A sudden impact to the chest due to a collision or from a moving object can also result in commotio cordis, or agitation of the heart, that leads to VFib. Also consider the H's and T's for other potential reversible causes.
Pro Tip #2: The H's and T's of PALS/ACLS is a mnemonic used to help recall the major contributing factors to pulseless arrest including pulseless electrical activity (PEA), Asystole, VFib, and V-tach. (In the next lesson – Asystole – we'll provide some more information on those H's and T's.)
The survival rate and outcome of patients with VFib or pulseless V-tach, as the initial arrest rhythm, are generally better than those of patients presenting with asystole or PEA. And as mentioned above, the outcome can be improved by prompt recognition and with the administration of high-quality CPR and defibrillation.




