Note: Your progress in watching these videos WILL NOT be tracked. These training videos are the same videos you will experience when you take the full ProPALS program. You may begin the training for free at any time to start officially tracking your progress toward your certificate of completion.
The term asystole simply refers to an absence of ventricular activity, which means the patient will exhibit no discernible electrical activity on an ECG readout. In most cases, asystole is a lethal arrhythmia and survival is extremely rare.
In this lesson, we'll look at an ECG readout for a patient in asystole, tackle those H's and T's and provide some corresponding information about their diagnostic use, and at the end of the lesson, provide some information on the principles of management of pediatric arrhythmias.
Asystole is a cardiac standstill where there is no discernable electrical activity. It Is represented by a straight flat, or almost flat, line on an ECG.
Warning: However, do not rely on an ECG alone for your diagnosis of a child in cardiac arrest. It's a good idea to always confirm it clinically, because what appears to be a flat line on the ECG, can also be caused by a loose ECG lead.
Now let's take a look at an ECG for a patient in asystole.
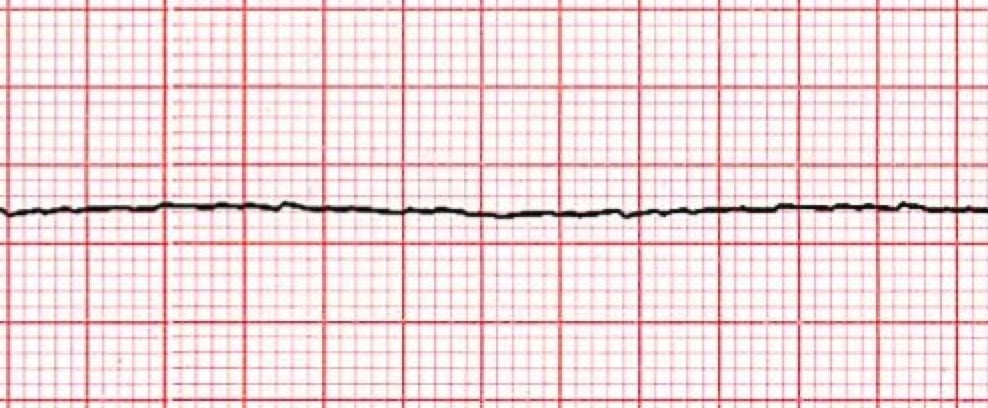
*Asystole ECG
1. The Heart Rhythm
The first thing you'll want to look at is the heart rhythm. Does the heart rhythm look regular? Or does it look irregular? In the ECG above, there is no heart rhythm.
2. The Heart Rate
Next, you'll want to look at the heart rate of the patient. What is the patient's heart rate? Is it normal? Or is it too slow or too fast? In this case, there is no rate and no pulse.
3. P-Wave
After looking at the heart rate, check to see if the patient's P-waves look normal by asking yourself the following few questions.
- Are the patient's P-waves present? No, making any other questions about QRS non-applicable
4. PR Interval
Next, look at the PR interval on the patient's ECG readout and ask yourself the following questions:
- Is the PR interval normal, meaning less than .20 seconds or is it contained within one large square on the readout? The answer is no, because there isn't a PR interval.
- Is the PR interval constant? Again, this in non-applicable since there isn't a P-wave.
5. QRS Complex
The last thing you should look at to determine if the sinus rhythm is normal or not is the QRS complex and ask yourself these questions while you do:
- Is the QRS interval less than .09 seconds? No. In fact, there is no evidence of a QRS complex, making any other questions about QRS non-applicable.
So, what is your cardiac interpretation? Based on these questions and on the findings from the ECG readout above, it would appear that this patient is in asystole. Because there is no myocardial, electrical, or mechanical activity, there is no pulse and no circulation of blood and oxygen.
Pro Tip #1: Asystole is most commonly seen following a period of unconverted ventricular fibrillations or ventricular tachycardia. And particularly in pediatric patients, hypoxia and shock can lead to asystole without appropriate and immediate intervention.
The most common reversible causes of asystole can best be remembered by keeping in mind the H's and T's.
H's and T's
Cardiac arrest in pediatric patients is often associated with a reversible condition. However, you're likely to miss one of them, if you don't make a conscious effort to think about reversible causes or complicating factors when assessing a child with cardiac complications.
The following H's and T's are designed to help you identify (and easily remember) potentially reversible causes of cardiac arrest in children or factors that may be complicating your resuscitative efforts.
The H's |
The T's |
| Hypothermia | Toxins |
| Hyper or hypokalemia | Tamponade |
| Hypoxia | Tension pneumothorax |
| Hydrogen ion (acidosis) | Thrombosis (pulmonary) |
| Hypovolemia | Thrombosis (coronary) |
Pro Tip #2: It's also important to consider unrecognized trauma, such as abdominal injuries and hemorrhage, as a potential cause of pediatric cardiac arrest, particularly when assessing and treating infants and younger children.
A Word About Principles of Management of Pediatric Arrhythmias
This will be a brief Word, but it could also be an important one.
Whenever a pediatric patient has an abnormal heart rate or rhythm, you'll need to quickly determine if that arrhythmia is causing hemodynamic instability or other signs of deterioration. The signs of instability in a child with arrhythmia include the following:
- Respiratory distress or failure
- Shock with poor end-organ perfusion, which may occur with or without hypotension
- Irritability or a decreased level of consciousness
- Chest pain or a vague feeling of discomfort in older children
- Sudden collapse
Your priorities during the initial management of arrhythmias are the same as they would be for all critically ill pediatric patients – support the ABCs first (airway, breathing, and circulation) and then treat the underlying cause.




